When it is found that your painful tooth has deep decay or fracture, usually root canal treatment maybe recommended. Appropriate radiographs or X rays as necessary for this decision. For better understanding of the internal structure or anatomy of the dental pulp and root canal, one should take the benefit of a 3D CBCT scan. This facilitates a better visualization of the root canal system.
The process of root canal treatment involves removing the infected pulp tissue and decay in the tooth following which the tooth will no longer be vital. You can learn the process of root canal treatments to understand the basics of the steps involved.
In the majority of patients, after the treatment is performed, the pain diminishes over 2-3 days. However, there might be a couple of reasons why the pain may persist even after that time. It might even worsen after the treatment, or recur over the next few weeks, months, or even years. Ideally, the tooth shouldn’t pain if the root canals have been cleaned and residual tissue removed completely and then filled after the tooth is made completely free of bacteria and infection.
Despite the high success rate of endodontic treatment being 86 – 98%, failures do occur in a large number of cases and most of the times can be attributed to the causes below. With an ever-increasing number of endodontic treatments being done each day, you should know the most fundamental of reasons leading to endodontic failure.
Here are the main reasons which might cause your tooth to still pain after a root canal treatment:
1. Anatomy of the dental pulp and root canals
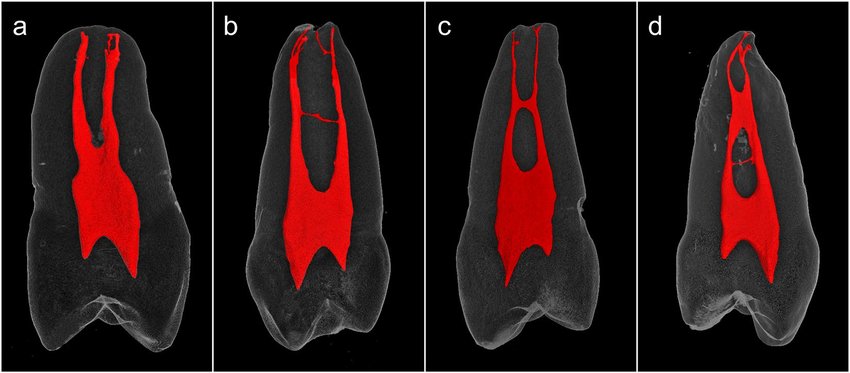
The root canal anatomy is quite complex with convergence and divergence of the canals at various levels of the root. This anatomy is only predictable to the extent of knowing the number of canals in the tooth that need to be filled.
However, there are accessory and lateral canals that aren’t visible on a 2D Xray and aren’t always possible to fill. Root canal treatments can also be performed under an endodontic microscope and/ or need to be observed under a Dental CT Scan for higher precision.
Intracanal branching and fusion are more of a norm in root canal configuration than the exception. Shaping and sealing of such root canals which are closely related and have ramifications, represent a special challenge for the clinician and are very often an almost insolvable task.
2. Failure to follow up
One of the more common reasons for root canal failure is if you have not completed the treatment and it has been left midway. For example, the root canal has been cleaned but hasn’t been filled yet or the root canals have been filled but the crown hasn’t been cemented onto the tooth for reinforcing the tooth.
It might occur due to the negligence of the patient and failure to return for treatment completion or could be the negligence of the doctor. None the less, this is a crucial step towards completing the procedure.
In such a case, the tooth might undergo micro fractures and lead to microleakage into the root canals overtime creating a communication between the oral cavity and the bone surrounding the roots eventually causing infection and pain.
In extreme cases, the tooth might even get fractured despite a successful root canal due to the failure of crown cementation on the tooth which brings us to the next point.
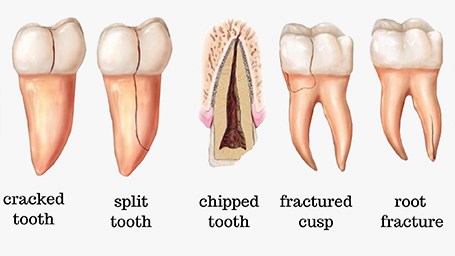
3. Fracture of the tooth
A more frustrating complication of root canal treatment is a vertical root fracture. Root canal treatment may lead to the tooth becoming more brittle especially if the tooth was severely decayed and there was significant loss of tooth material involved to save the tooth (source)
It can also occur if the tooth was bearing direct forces of chewing without having a dental crown cemented onto it after completion of the root canal treatment.
It is often difficult to diagnose as the tooth may appear healthy on 2D X rays (radiographic examination). With limited diagnostics, it may appear that re-root canal will be a solution, however, a high-resolution dental CT scan will be more effective to identify the fine fracture lines.
It may manifest as constant throbbing pain which may not be completely relieved with medication. In the case of vertical root fracture, the affected root or tooth has an unfavorable prognosis, and extraction is usually the only treatment option.
4. Under filling or Overfilling of root canals
Apart from proper cleaning and disinfection of the canals, a key factor is the quality of filling done in the canals. The quality of root canal filling plays a major role in determining the success of the treatment. In cases with root canal failures, 65% of the cases exhibited poor quality filling whereas 42% of the teeth had some canals which were left untreated.

Also, an overextended filling is 4 times more likely to fail than under obturated canals. The success rates of root canals are significantly lower if the filling overextends the root apex by 2mm or flushes with the root tip. Ideally, it must be a .5 mm short of the root tip.
In under and overextended root canal fillings, there is an increased incidence of infection around the root in the bone. Usually, underfilled root canals can be retreated. Overfilled canals can be retreated as well if the extension is up to 2mm. Beyond that will require a minor oral surgical procedure called Apicectomy where the root tips are surgically reduced and surrounding infection is removed.
In the case of second molars and/ or third molars, the painful tooth should be extracted if the canals are excessively overfilled.

5. Incomplete removal of decay or occurrence of secondary decay
Sometimes new decay can expose the root canal filling material to bacteria, causing a new infection in the tooth. This may occur if the decay or cavities in the tooth were not completely removed during the root canal procedure. Since the decay persists, it continues to destroy organic tooth structure and creates toxins which may result in failure of the root canal and subsequent pain.
It may also occur due to open margins between the crown and the tooth structure if the crown preparation isn’t done appropriately or the crown doesn’t have a seamless margin with the prepared tooth.


Decay under the crown is circled in red
The tooth can be retreated but there are high chances of the tooth breaking/ fracturing when the crown is removed. Extraction of the tooth might be the only solution left in that occurrence.
6. Missed canal orifices
In this study (https://pubmed.ncbi.nlm.nih.gov/23930451/) Missed canals were identified in 64 of the 133 previously treated teeth (48%). Of the total missed canals, 11% involved a maxillary second molar and 44% involved a maxillary first molar.
This occurs mostly since these teeth deviate the most from typical tooth anatomy and have a lot of variations, meaning, there could be additional root canals in the tooth which are much smaller and harder to see on a 2 D Xray so they are more likely to be missed.
These are equally difficult to visualize and treat under a high-resolution dental microscope.

The above X ray clearly shows that the third root has been completely missed.
Given that failure to locate all the canals of a tooth contributes significantly to unsuccessful endodontic treatment, all measures available to maximize canal identification should be used.
A 3D CBCT high-resolution scan is very useful in such cases to accurately find the exact number of canals and where they are located in the tooth.
7. Iatrogenic causes:
This implies the causes of tooth pain after root canal treatment due to the clinician. Improper root canal orifice exploration may cause perforation of the tooth. Sometimes in case of severely inclined or angulated roots, there is a chance of deviation from the normal anatomy of the tooth leading to perforation of the canal.
Other iatrogenic causes include excessive widening of the canals, transportation of the apex of the root, and breakage of the fine dental files within the root canal. Since root canal treatment is more or less a blind procedure as the interior of the canals isn’t visible during treatment, root canals that are harder to navigate are more likely to suffer from such issues.
Severe angulation in roots curving backwards

Transportation of apex of the root

Broken file extending through the canal apex

8. Neighboring teeth causing persisting pain
I would like to share a case study:
A patient complained of constant dull pain around the left lower side of her jaw which had become extremely painful since two weeks. On examination, it was observed that her second and third molar had dental issues. The second molar had a deep cavity and the third molar was decayed and hadn’t completely erupted.
The pain was radiating to her forehead and neck and all teeth on that side were painful. It was clear that both teeth had to be treated and she was advised about the same.
The second molar was root canal treated but the pain persisted. Soon after her root canal, the third molar was extracted following which she experienced a rapid reduction in her pain over the next week and she has been asymptomatic since then.
This only goes to prove that if multiple teeth are damaged, they all need to be treated for complete relief from pain and further complications.

Conclusion
Although root canal treatments are largely successful, there might be several causes for failure of the procedure and recurrence of pain. It is essential to diagnose the issue accurately before proceeding with any treatment. This article must have helped you to learn more about the possibilities so you can be more aware of the cause of the pain and solutions that are available.


